Leadership for Successful Electronic Medical Record Implementation: A lesson learned at a health facility in Ethiopia
It has been a couple of months since the Ministry of Health (MOH) turned its attention towards improving point of care applications to ensure quality of care, universal health coverage, and equity. Electronic Medical Records (EMR) system is one of the digital tools used to digitalize workflows within health facilities, becoming one of MOH’s flagship digital tools.
Ethiopia has been trying to implement EMR at public health facilities for many years. Efforts, however, have been unsuccessful in all but a few facilities. The main reasons for failure were that there was no national EMR implementation roadmap that guides the overall EMR implementation, absence of EHR standard that governs the tools and EMR compliant site selection, health facilities management poor attitude towards EMR implementation, expensive investment requirement and lack of priority by the Ministry of Health are to be mentioned among many. This has taught MOH as well as EMR implementers that EMR implementation is beyond scaling technology and has different characteristics than other health information system tools. Over the past few months, the Digital Health Activity (DHA) has been supporting the MOH with EMR implementation at selected health facilities.
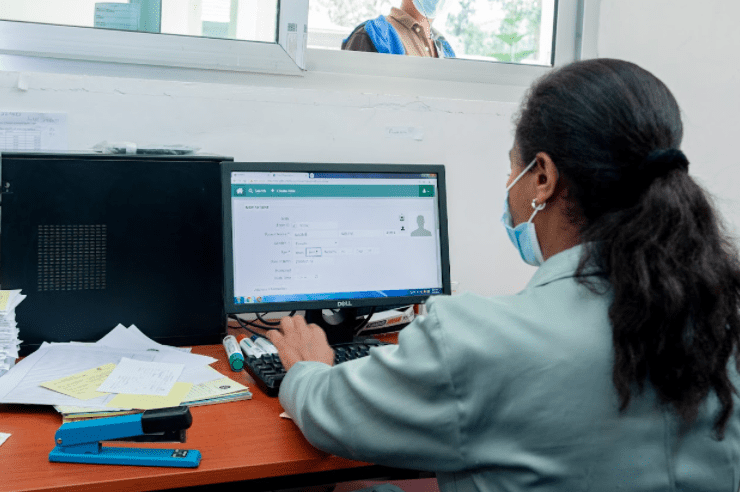
The system deployed at these health facilities is Bahmni, a global open EMR tool that meets the Ethiopian Electronic Health Record (EHR) standard and provides end-to-end automation of health facility services. Implementation of EMR in a hospital takes more time than a health center because the volume of services is far higher at hospitals. Implementation at one of the hospitals started in mid-2019 and involved infrastructure fulfillment, equipment procurement, and provision of on-the-job training. DHA documented challenges and lessons identified over the course of implementation to inform subsequent EMR scale up efforts. Among the challenges were leadership and staff attitude to use EMR, Business Process Reengineering (BPR), and frequent changes in service delivery rooms due to COVID-19. DHA has worked closely and aggressively with the management and the staff to overcome these challenges.
EMR scale-up in three health centers started in July 2021. A set of predefined criteria was used to select the health centers in Addis Ababa. Comparatively to the hospital, the implementation progressed rapidly, with many of the service delivery rooms implementing the EMR in a short period of time.
Ferensay health center is one of the champions in implementing the EMR within a short time in all of its eight outpatient departments and laboratory unit. DHA provided on-the-job training while the health center leadership secured the necessary infrastructure and equipment and changed staff attitudes about the use of EMR by building an understanding of its benefit to service quality. In a gesture of commitment, the CEO and medical director even gave their own desktop computers to service delivery rooms to fill the infrastructure gap.
The implementation of EMR at Ferensay health center can be considered as a “True Implementation”, as the implementation is growth-oriented and sustainable. The implementation is natural, internalized by the staff and grows to other delivery rooms, and strives to digitize a system end to end. The health management information system (HMIS) team head looks forward to when the EMR is interoperable with DHIS2 to end the tiresome process of tallying reports from each delivery room and to improve data quality. This showed that the staff’s understanding about digitization is allowing them to push the implementation forward and move ahead of the implementers.
When clinicians reported that patients were offended because they thought they were not getting full attention when clinicians used EMR on their mobile phones or computers, Ferensay started educating patients about the benefits of EMR through a health education program for the community. This has helped to improve the patients’ acceptability of EMR which will contribute to the success of scale-up efforts, and shows the impact of community engagement in the success of EMR implementation.
The major lesson from EMR implementation is that leadership support and favorable staff attitude are critical. Facility management with an open mindset and attitude about digitization can facilitate full automation of EMR even if there is poor infrastructure. Infrastructure gaps can be closed with partner and stakeholder resource mobilization. Facilities eager to implement EMR should consider training staff first to ensure understanding and acceptance.
Article by:

Digitalization Director, USAID Digital Health Activity
