Considering Interoperability and Governance in the Expansion of Digital Health

Digitization Director, USAID Digital Health Activity
At JSI, and across the field of public health, we are persistently seeking tools to optimize health programming. Digital health technologies emerged as a path to progress in this pursuit. Their growing use cases have resulted in improved access to care among health care clients; reduction in redundancies, waste and cost; and growing opportunities for health worker skills building. There are a growing number of digital tools now in use across our supported health programs: from digitized client health records and telemedicine platforms to supply chain management tools. The applications seem limitless, but they come at a cost and require careful consideration, including financial; useability among health staff; how they should be governed, and, as they further expand across the health system, interoperability. We sat down with Biruhtesfa Abere, JSI’s Digitization Director of the USAID-funded Digital Health Activity (DHA) to learn more about what these investments can look like in practice and what he’s learned in recent years about their considerations.
Question: Why is digital health significant?
To date, we have seen digital health create standardization across health services and workflows, facilitate seamless communication among care professionals and their patients, and improve evidence-informed decision-making. In particular, over these last several years, the COVID-19 pandemic underscored these benefits. We’ve seen how telemedicine can save lives; how digital tooling has reinforced both reporting and referral systems, where we can strengthen the continuum of care, and how to optimize human resources for health, to name a few.
Question: How is the Digital Health Activity moving this area of work forward?
DHA is helping Ethiopia’s Ministry of Health achieve its goal of an Information Revolution: a complete digitization of the national health care system. DHA, among other projects, is working on the development and implementation of the electronic medical records (EMR) system and the electronic logistics management information system (eLMIS or Dagu).
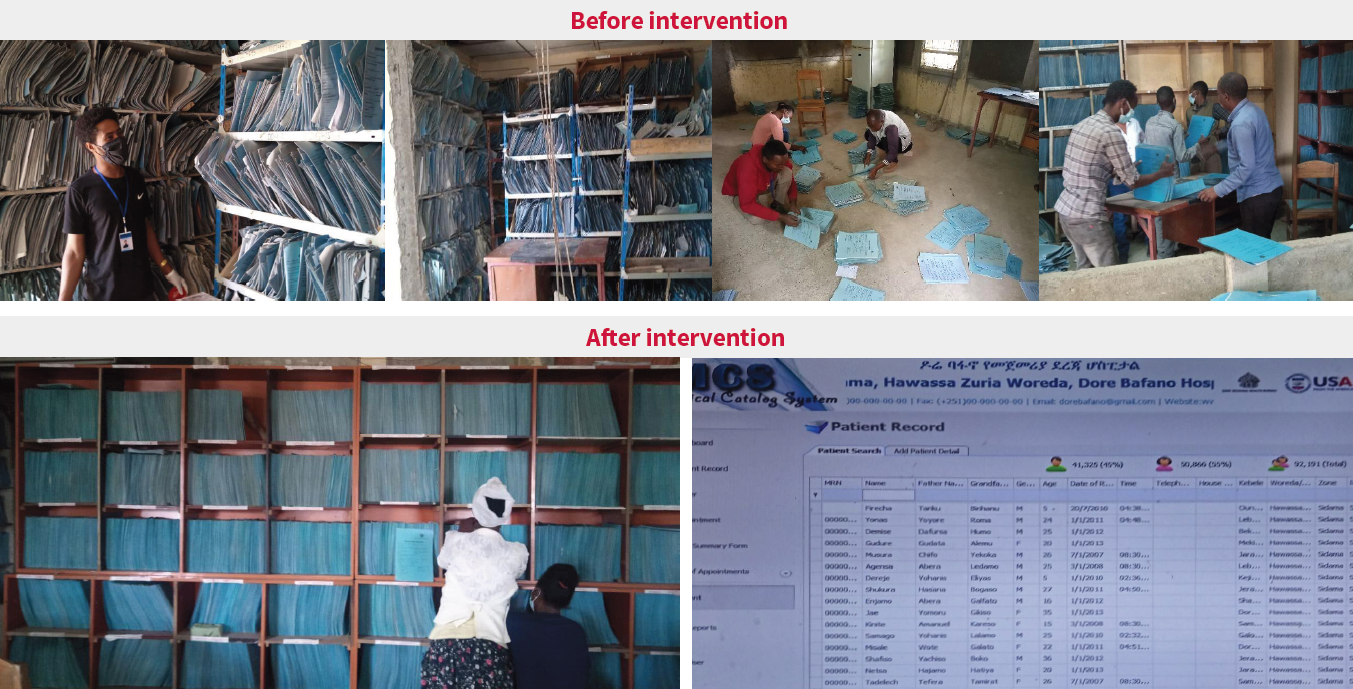
The EMR is an OpenMRS-based tool customized to a country’s clinical service guidelines. It automates health facilities workflows to enhance quality of care and ultimately improve patient health outcomes. EMR has shown significant changes in improving patient waiting time in health facilities, turnaround time in communicating diagnostic results to patients, decision support systems and more. This tool has enabled faster access to patient health records among health facility staff, allowing for quicker patient flow through hospital triage units. This time saved has led to lives saved.
The facility logistics management system, Dagu, is a locally developed health stock management system deployed at pharmaceutical stores of more than 1,139 health facilities. It is connected to supply chain systems at sub-national and national levels and enables health facilities to efficiently manage stock using real-time data, request refills and more. Dagu has enabled health facilities to reduce stock outs and properly manage expiry.
Question: Why is interoperability vital in digital health?
The implementation and adoption of multiple digital health solutions has also pushed the interoperability agenda to the forefront of all digital health discussions: if we’re building out all of these tools in isolation: how are we growing and learning from the high-quality and real-time data they’re collecting?
Interoperability connects all these systems, so that they are speaking to one another. Enabling sub-systems to exchange health related data, not only allows for greater automation in the healthcare system, but allows for a better flow of data for improved health program decision-making.
When health systems are integrated, what users gain is multiple systems that function as one for a single purpose and impact. For example, the interoperability of EMR and Dagu allowed for streamlined medication management wherein clinics are well stocked according to medication use history. As a result, health care service providers are now able to view the availability of a particular medication in the EMR, place orders for dispensing, and receive confirmation once the patient has received the prescribed medication. Additionally, pharmacists can seamlessly receive orders from the EMR and process them using the Dagu dispensing unit. These systems all speaking to one another creates this long string of data that can give a health worker treating a patient the full story of that patient’s care.
Question: How do we operationalize interoperability?
Mapping out tools, how they can exchange data from one another and then developing pathways for their own communication is how interoperability is generally put into practice. To facilitate interoperability, countries have introduced eHealth architecture: a blueprint for integrated digital systems. DHA uses eHealth architecture and its principles to guide interoperability among sub-systems. Developing interoperability in a health program environment has become easier, with healthcare software engineers adopting recommended standards and mediators to develop interoperability instead of traditional point-to-point integration methods.
Ministries of health and donors are also enforcing systems to develop interoperability and data exchange standards. As a result, subsystems are being developed by using standards like Fast Health Interoperability Resource (FHIR) to facilitate seamless data exchange among subsystems. OpenHIM was also used by DHA as a mediator (an interoperability layer that moderates data exchange) between systems in order to authenticate, encrypt, transform, queue, validate, and translate data. Both FHIR and OpenHIM are deployed in a server inside a data center within health facilities to avoid dependency on internet connectivity.

Question: What is needed for interoperability, and digital health more broadly, to succeed?
A reliable local area network infrastructure: The majority of facilities, at least those that we support through DHA, lack a well-established local area network, which is essential for the efficient deployment and utilization of systems and interoperability. Investing in infrastructure enables efficient exchange of data among digital tools and limits interruption and/or difficulty connecting to IT peripherals, lab machines, and other devices.
A dedicated data center is needed to avoid relying on internet connectivity. It is also recommended to deploy a system with its interoperability layer on premises, which requires a dedicated mini data center to be available at health facilities. Mini-data centers are typically smaller in scale compared to conventional data centers and house medium level computing equipment like servers, storage and networking devices. This enables system back-ups when internet connectivity is dropped.
IT equipment, like computers, tablets, etc. are crucial for enabling the use of digital health tools and establishing a platform for data flow. Often the equipment we’re using in public health, particularly in low- or middle-income countries, is outdated, malfunctioning, or lacks sufficient specifications. This not only impedes data exchange, but also obstructs successful implementation of digital tools in health care facilities, making it difficult for end-users to utilize the tools effectively.
Health information technology (HIT) specialists play a critical role in ensuring systems function smoothly. In instances where systems or mediators malfunction, human intervention is required to perform necessary maintenance. HITs, particularly those based at facility levels, provide prompt support and solutions to ensure speedy resolution. Failure to provide such support services can cause delays in restoring systems, interoperability, and services, resulting in frustration for end users, impeding adoption.
Question: How are health workers crucial in digital health?
The importance of health workers accepting digital tools cannot be overstated; it may even be more crucial than having the necessary equipment and infrastructure in the first place. Health workers’ digital literacy and acceptance are vital for the success of digital health innovations. While there is forward movement in educating health graduates on digital technologies, there remain gaps in building the competence of the health workforce in efficient utilization of technology.
Question: What are some of the priorities or areas of need that we should be paying special attention to as we continue to roll out digital health technologies?
While creating interoperability and demonstrating data exchange in a sandbox, or testing environment is uncomplicated, it is not the sole objective. The ultimate goal is to create a resilient, accessible and equitable health systems. Innovations and new technology can push us closer to this goal but only so long as we establish standardized data exchange: tools that are heighting our work in public health, that can feed off of one another and continuously expand quality and efficiency in health care. For this to happen, a methodological, organized approach to digital health infrastructure and governance practices should be at the forefront now.
To find out more about JSI’s digital health work click here, or sign up for newsletters here.